ExoSurge® Peyronie's Treatment Technology

Other Peyronie's questions?
What is ExoSurge technology and how does it work?
ExoSurge technology was born from over twenty years of focused research and collaborations. The first decade was dedicated mostly to uncovering what actually causes Peyronie’s (the epidemiology of Peyronie’s disease). We hypothesized we were unlikely to find a curative solution to the problem until we understood exactly what the problem was.
It’s long been hypothesized Peyronie’s is caused by penile trauma but that never explained many cases, including the most common version where otherwise perfectly healthy men simply awake with an ugly curve during morning erections. The ExoSurge team unlocked those secrets. Subsequently, they had to develop a treatment technology that could effectively remove the penile fibrous plaques that cause all Peyronie’s awful symptoms. Peyronie’s fibrosis is embedded in the penile neurovascular nerve bundle, making it impossible to effectively remove surgically without causing tremendous risk to lost sensation.
Following is an encapsulation of this new Peyronie’s technology.
ExoSurge® Inter-fibrinous Pulsated Gas and Drug Technology (IPG)
Introducing a paradigm-shift approach to treatment of Peyronie’s Disease.

How does ExoSurge work?
ExoSurge is a tandem of treatments guided by a detailed algorithm that results in safe dissolution of Peyronie’s fibrous plaques, which are the underlying source for the nasty symptoms Peyronie’s is famous for.
The key workhorse of this technology is the patented IPG pulsated gas injections which allow injected drugs to properly penetrate dense fibrous plaques and begin dissolution. In some cases (20%), we prescribe therapies to induce increased penile blood flow (if it’s found to be deficient) during ultrasound testing. All patients are put on regimens to optimize and improve their scoring with “Peyronie’s Accelerators”. Otherwise, the removal of fibrous plaques can be incredibly slow since the body is suited to add more when these metrics are out of alignment.
Eight issued patents, 18 patents and provisionals filed both nationally and internationally

The ExoSurge Treatment Device
Our patented and clinically proven ExoSurge® method permanently removes fibrous tissue plaques linked to a Peyronie’s Disease diagnosis by using injected and pulsating gases in conjunction with intralesional medication injections.
A device roughly 24 inches wide by four feet tall that is mounted on rollers is used to administer these gas injections. As so, it may be rolled into place and stored in an exam room corner while patients are being treated. Before therapy starts, an initial assessment of the case dynamics is conducted, and interlesional injections of Trental, Verapamil, or both may be administered in combination with ExoSurge therapies.
The most frequent adverse effect is mild redness in the treated area, and treatments are well tolerated, taking approximately 15 to 20 minutes to complete. A single ExoSurge treatment per day is permitted for a patient.

What effects will this revolutionary ExoSurge technology have on Peyronie’s patients?
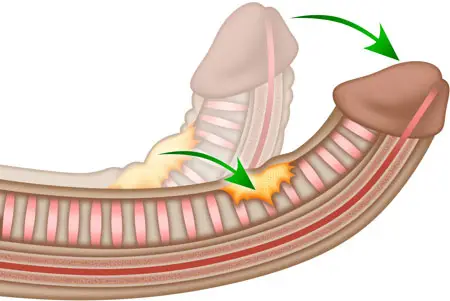
Erection-related penile curvature is a common indication of Peyronie’s disease. More than 60% of Peyronie’s cases include significant bending. The reason it happens most frequently is that the fibrous plaques that produce Peyronie’s symptoms typically develop along the tunica albuginea, which is the thick sheath that divides the erection tissue within the penis organ. If the left side of the tunica is where the majority of this fibrous plaque accumulation happens? When the penis is erect, it will curve to the left and, conversely, to the right. The degree of curvature is more prominent the larger the fibrous mass along the tunica.
However, curvature is only one of several common symptoms. It is not the root cause or definition of the condition.
When a disease remains incurable for centuries, its symptoms almost always become society’s definition of that disease.
Similarly, the efficacy of the treatments is measured by how well the symptoms are alleviated.
For example, this phenomenon is exemplified by the common cold. Coughing, sneezing, runny nose, sore throat and congestion are the most common symptoms, and people immediately assume we have a cold if we display these symptoms. Nobody inquiries about the type of virus we are fighting, such as rhinovirus, coronavirus, adenovirus, or enterovirus.
Since Peyronie’s Disease has remained similarly incurable, it has likewise become only known for its symptoms, even among many physicians, with erect curvature being the most notable definition. Thus, every approved treatment and medication for Peyronies is evaluated solely based on its efficacy in reducing erect curvature.

This is what makes ExoSurge® completely different from anything ever used to treat Peyronie’s.
ExoSurge® technology treats, heals and cures the underlying disease of Peyronie’s, not just its symptoms.
ExoSurge® is the world’s first clinically-proven treatment to conservatively and permanently remove plaques and fibrosis associated with a Peyronie’s diagnosis.
Our philosophy
Our clinic is focused on finding a cure for Peyronie’s Disease. After more than two decades of research and development, we’ve achieved many major milestones in pursuit of our purpose, including:
- We identified the underlying epidemiology of Peyronie’s.
- Our research identified six Peyronie’s Accelerators that need to be regulated and optimized to treat the disease.
- Our patented therapeutic uses pulsated gas injections to penetrate Peyronie’s fibrous plaques, allowing medications to breakdown fibrosis without surgery.
- Our new therapy algorithm takes into account all variables of a Peyronie’s case, such as plaque size, density, and position, as well as health factor rating and the state of each Peyronie’s Accelerator. This will assist future clinicians in treating cases.
Earlier in our Peyronie’s technology development, we were unable to restore the original size of the penis following the removal of Peyronie’s plaques, therefore we developed unique approaches for cosmetic urology (penis augmentation). Since then, we’ve learned ways to restore lost size from Peyronie’s during therapeutic treatments, but our cosmetic urology platform, led by renowned reconstructive urologist Kenneth J. Carney, MD, PHARM, FACS, has been highly successful. Our cosmetic platform has provided the principal funding for our Peyronie’s research.
We are now developing technology to accelerate the progression of obstinate Peyronie’s cases using enhanced techniques and innovative medications. We have initiated negotiations to partner with a multinational pharmaceutical platform to fund our FDA approvals and help ensure the ExoSurge breakthrough is available internationally in the coming years.

