Peyronie's Surgery: Important New Advancement Adjunct with ExoSurge®
Peyronie’s Surgery: Major New Advancement
When Kenneth Jeffery Carney, MD PharmD joined our institute as Chief medical Officer after leaving Emory, he viewed ExoSurge in a somewhat different light that our technology’s primary inventor, Steven L. Morganstern, MD. Whereas Dr. Morganstern’s vision with Peyronie’s care was a complete conservative solution, Dr. Carney began exploring ideas where ExoSurge technology could be used adjunctively with surgery to create faster and improved outcomes for severe cases.
While this version Of ExoSurge technology is still under development, Dr. Carney was able to successfully perform a Peyronie’s plication procedure without any loss of penile length as an adjunct to ExoSurge therapy. Peyronie’s plication has long been established as the surgery with the least likelihood of post-surgical complications when it comes to penile function and sensation, but it sometimes results in substantialness of penile length. This new adjunctive track could help change all of that.
When this test patient first arrived for care, he presented with 80 degree erect curvature, with long established, large, and dense fibrous plaques in both calcified and non-calcified states.
ExoSurge technology and protocols were able to removes plaques and reduce the patient’s erect curvature to about thirty degrees. Dr. Carney then employed plication surgery which resulted in complete restoration of pre-Peyronie’s penile length and girth and a totally straight penis.
We believe this new pathway might be a valuable option for our urology clinician partners in the future.

Existing Peyronie’s Surgery Techniques
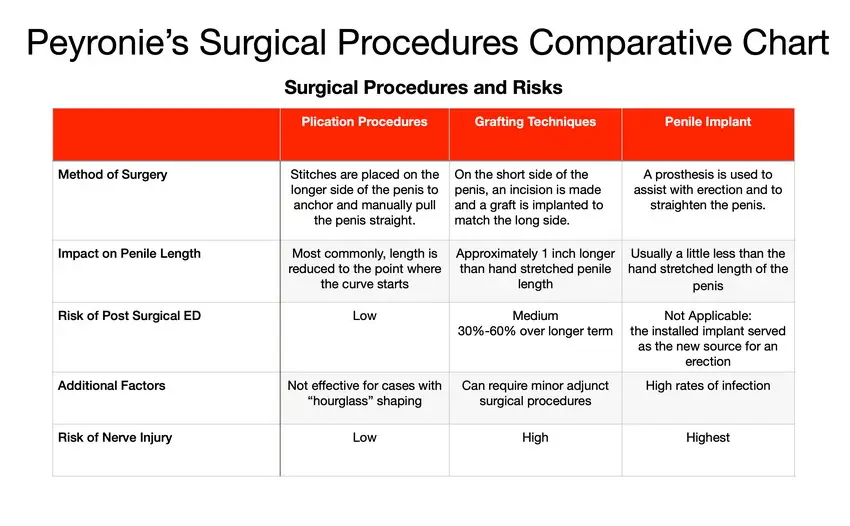
Current AUA (American Urology Association) guidelines recommend the following Peyronie’s surgeries as possible solution pathways for patients
- Plication Surgery: In this procedure, the penis is straightened straightened, extra tissue on the formerly outer side of the curve cinched together using a sequence of sutures, or “tucks.” The length of the shorter side, or the side with the Peyronie disease scar, will determine the final penile length, which is usually shorter than before.
- Incision and grafting techniques: In this case, surgeons incise within the plaque at the point where the curvature starts and add a graft synthetic or biological material to replace this area. to straighten the penis. Primary complaint is loss of sensation and erectile dysfunction.
- Penile implant with Peyronie’s Surgery: In cases of severe erectile dysfunction and severe Peyronie’s disease, the implant pathway includes curvature straightening combined with installation of a penile prosthesis.
Plication Surgery for Peyronie’s Disease
Generally, plication surgery is most commonly recommended when erect penile curvature is less than 60 degrees.
Penile straightening is accomplished by implanting a surgical suture on the convex side of the curve, which is then used as an anchor to manually realign the curve. Despite the fact that the Nesbit procedure1 is the most well-known plication technique, a number of improvised variants are currently more prevalent. The primary adverse effect of plication is penile erect shortening; the more severe the curvature, the more pronounced the postoperative penile shortening2. Penile curvatures greater than sixty degrees have a tendency to exacerbate the penile shortening effect following plication, making it rarely used in those cases.
Incision and Grafting Surgery for Peyronie’s
Most urologists recommend a grating technique for patients whose erect curvature exceeds 60 degrees3. Some surgeons recommend it for patients below 60 degrees whose erection length is markedly shorter than average, as the lost length from plication often renders the patient too short to engage in sexual activity. Most grating procedures entail a partial or complete incision into the Peyronie’s plaque penile at its most pronounced point of curvature. By extending the concave side of the penile curvature, this method of penile elongation reduces the risk of penile shortening. The incision made during Peyronie’s grafting leaves a section of the tunica albuginea open, which is then filled with various autologous or non-autologous grafts4.
Grafting surgical procedures are more complicated than plication because extensive dissection and elevation of the neurovascular bundle within Buck’s fascia are required. It’s also why there’s a more common occurrence of post-surgical erectile dysfunction with graft techniques versus plication.
Some patients mistakenly believe that this procedure involves surgical removal of the Peyronie’s plaque. Peyronie’s plaque is embedded within the penile neurovascular bundle, the “electrical operating system” for the sensation, function, and delight of the penile organ. Earlier attempts to eradicate the majority of the plaque resulted in a high prevalence of severe erectile dysfunction. That is no longer advised.
[1] Zargooshi J. Trauma as the cause of Peyronie’s disease: Penile fracture as a model of trauma. J Urol 2004;172:186-8.
[2] Greenfield J.M., Lucas S., Levine L.A. (2006) Factors affecting the loss of length associated with tunica albuginea plication for correction of penile curvature. J Urol 175: 238–241
[3] Hatzichristodoulou G, Gschwend JE, Lahme S. Surgical therapy of Peyronie’s disease by partial plaque excision and grafting with collagen fleece: feasibility study of a new technique. Int J Impot Res 2013;25:183-7.
Penile Prosthetic Implant Peyronie’s Surgery
Patients with severe and chronic ED plus a severe Peyronie’s disease diagnosis are prospective candidates for treatment with prosthetic implants5. During surgery, the prosthesis is implanted, and the penis is “molded” in order to straighten it, while the prosthesis is distended to correct the curvature. Even if this does not completely correct the curvature, prolonged use of the prosthesis typically does so.
Proper patient education regarding the dangers of penile shortening and/or deformity is required by medical standards. Detailed patient assessment and counselling are necessary to ensure that patients have realistic expectations and to mitigate potential increased complications
[4] Levine LA. Partial plaque excision and grafting (PEG) for Peyronie’s disease. J Sex Med 2011;8:1842-5.
[5] Levine LA, Dimitrou RJ. A surgical algorithm for penile prosthesis placement in men with erectile failure and Peyronie’s disease. Int J Impot Res 2000;12:147-51.
associated with Peyronie’s-related procedures, such as an increased risk of intraoperative crossover, corporal or urethral perforation, or the need for a smaller prosthetic6.
Peyronie’s Surgery Procedures Compared
Peyronie’s Surgery: Long Term Success and Failures Studies
Almost every study regarding improvement band patient satisfaction from Peyronie’s surgery only includes approximately two years of follow-up analysis.
The results of the first-ever retrospective analysis on the long-term efficacy of Peyronie’s disease surgery to treat the disease, which was
[6] Sansalone S, Garaffa G, Djinovic R, et al. Simultaneous penile lengthening and penile prosthesis implantation in patients with Peyronie’s disease, refractory erectile dysfunction, and severe penile shortening. J Sex Med 2012;9:316-21.
published in 2012, were dismal. According to a recent retrospective study published in 2012 by Florian Wimpissinger, MD, of the department of urology at Rudolfstiftung Hospital in Vienna, Austria regarding the long-term results of PD surgery, the outcomes are far from optimal.
After a mean of 9.3 years, the recurrence of postoperative curvature increased from 0% to 23.7%, post-op erectile dysfunction increased from 3.0% to 39.5%, penile shortening increased from 0% to 65.8%, and impairment of penile sensitivity increased from 3% to 31.3%.
Dr. Wimpissinger, who presented the study’s findings at the annual meeting of the European Association of Urology in Vienna in 2011, observed that “results tend to deteriorate over time.” Dr. Wimpissinger stated, “Since these results were significantly better during the first few months or years after surgery, it can be assumed that all of these aspects are due to the chronic/recurring nature of PD.”
Dr. Wimpissinger stated that all published data on the outcomes of PD surgery must be interpreted differently based on the findings of a lengthy follow-up.
In other words?
Long-term surgical outcomes indicate that the condition frequently returns and becomes equally debilitating and excruciating.

