Major Peyronie’s Treatment Breakthrough

Morganstern Urology and its sibling company EXO Biomedical have been working to find a cure for Peyronie’s Disease for the past twenty years. This medical procedure innovation couldn’t be more pertinent.
How common is Peyronie’s Disease? The prevalence of the Peyronie’s Disease condition among American men 30 years of age and younger has increased by 600%, according to recently published studies. According to the National Institute of Health, approximately 1% of all men 19 and older have been diagnosed with Peyronie’s Disease. This does not include counting the men who have the symptoms, yet have not a medical diagnosis.
It is clear that a Peyronie’s indication could become epidemic in the next 15 to 20 years, with incidence rates potentially exceeding 20% of all US men, if we take into account the historical incidence of acute penile trauma (accidents) on this basis and other issues we discovered by determining the etiology of the disease.
Uncovering the precise etiology of Peyronie’s took up over half the time it required to make this significant breakthrough. Although there were various theories as to why this disease occurs, none could account for every occurrence. It was frustrating to finish that process.
The plaque and fibrosis can now be completely removed from every case we come across among compliant patients. Since complex cases can be more time-consuming, our current focus is on inventing new approaches that cause results to happen faster.
In the next two years, we intend to collaborate with a major pharmaceutical company to provide our discovery to men all over the world, and we believe that our solution will be covered by health insurance. Unfortunately, the $20 million we have spent to date developing, testing, and perfecting this ground-breaking discovery will pale in comparison to costs of regulatory clearance and scale-up connected with our technology. We cannot afford to go this alone.
Similar to that, there are many aspects of our technology that we cannot openly reveal. To entice the most suitable Pharma partner, we are required to guard aspects of our pending patents.
Request Information
Why isn’t ExoSurge being discussed by other urologists? Although we haven’t yet published, we will start disclosing additional information later in 2023. Though we think you’ll soon start seeing and hearing a lot more about our innovation, our lawyers have advised that many crucial aspects must be kept a secret for the time being.
We are aware of the large number of individuals suffering from Peyronie’s disease all across the country who are unable to pay the travel and treatment expenses to receive care at our facility in Atlanta. These men and those who have endured this terrible disease for a long time are the inspiration of our two decades of work and present focus.
What Causes Peyronie’s Disease?

Have you ever searched “What causes Peyronie’s Disease?”
Nobody knows for sure.
Peyronie’s disease was named after Louis XV’s personal physician, Francois De La Peyronie, who produced a treatise on the subject in 1743. (He had the condition himself). The symptoms, however, have been documented in medical publications since the Middle Ages.
Can you think of another disease that has been clinically recognized for over 600 years but has such a limited etiology?
There are ideas, most of which are related to penile trauma, but none can effectively explain why symptoms occur suddenly and without warning in the majority of cases in otherwise completely healthy males.
How can you find an innovative solution if you don’t know the root cause of the problem?
Where traditional Peyronie’s Care went wrong

Targeting the wrong problems
Why have so many attempts at a Peyronie’s solutions fallen flat? We believe it’s because they targeted the wrong problem.
Every traditional Peyronie’s care approach appears to have been invented using the concept that problem-solving equals invention. In other words, the penis becomes distorted from Peyronie’s in size or shape while it is erect, which is the Peyronie’s “problem”.
That would seem to imply…
If I manually straighten my Peyronie’s curvature through force with a traction device but the plaque that caused the curvature is still inside my penis, am I cured?
I’m good to go if my doctor injects a potent collagenase or enzymatic mixture into my penile plaque, softening it enough to physically straighten my organ?
Also, what about the numerous instances of Peyronie’s plaque and fibrosis in males who don’t exhibit these symptoms? The majority of such patients stated that they were often questioned about how “inconvenient” the problem was for them, even as their penile performance continued to decline.
Is it true that these latter patients do not have Peyronie’s Disease?
The Pathway to a Peyronie’s Cure: Symptoms
You cannot solve what you don’t understand.
The “problem” to be solved before developing an innovative medical procedure to cure Peyronie’s Disease was never within treating its many symptoms.
What are the symptoms of Peyronie’s Disease?
Symptoms include erect curvature, lost length, shaft indentions when engorged, lost sensation and erectile dysfunction.
The root problem is “What causes Peyronie’s Disease?”
How could we develop a permanent solution to healing Peyronie’s disease if we didn’t understand the details surrounding its underlying etiology? We didn’t think that was possible. We also felt this was the reason existing treatments came up short: they all medical procedures provided solutions to treat various Peyronie’s symptoms, never the removal of the basis for the disease itself.
During our twenty-year odyssey developing our breakthrough technology that permanently removes the fibrosis and penile plaques that trigger a Peyronie’s diagnosis, we found it imperative to develop a “working theory” regarding the etiology of Peyronie’s Disease.
Those working theories were mailable early on but became static over the last seven years as our technology began to prove effectual.
Our working hypothesis regarding the etiology of Peyronie’s Disease is multi-faceted and includes case and patient specific variables. It will require numerous future studies to achieve enhanced clinical accuracy.
However, we’ve reached a point using our working theory method in tandem with our treatment devices and protocols where, all, meaning 100% of Peyronie’s patients who are compliant and complete treatment with our technology see permanent reduction in penile fibrosis and plaques.
Why Does Peyronie’s Disease Occur?
Answered: What Causes Peyronie’s Disease?

We’ve determined Peyronie’s disease is caused from a wide variety of sources of penile trauma1. The existence of ten unique “Peyronie’s Accelerators” cause a benign case to evolve to a problematic Peyronie’s diagnosis, often without warning. There are ten different manifestations of plaque formations within the soft tissue of the penis that exhibit as “Peyronie’s Disease”, each requires a customized approach for removal. Finally, select “predisposed” patients are much more prone to build up fibrosis equating to a Peyronie’s diagnosis even after only a singular microtrauma. These later examples would fall into the category of “wound healing disorder,” which is still widely used to define the disease, but these cases are far less prevalent.
[1] Zargooshi J. Trauma as the cause of Peyronie’s disease: Penile fracture as a model of trauma. J Urol 2004;172:186-8.
[2] The pathophysiology of Peyronie’s disease: beyond the Smith’s space Int Braz J Urol, 41 (2015), pp. 1040-1042
Introduction to Peyronie’s Disease
Before We Get Started: Penile Function 101

Before we enlighten you on many new realities and observations concerning Peyronie’s Disease, it’s critical to highlight the major portions of your penis that are most immediately affected by the disease.
Three Basic Functions
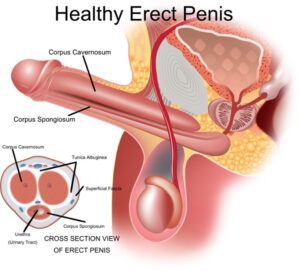
Your penis serves three essential purposes. The corpora cavernosa, a pair of thick “sponges” along the top that become fully engorged with blood following sexual arousal, is most men’s favorite penile trait. These tubes are stiff enough to allow vaginal penetration during sexual intercourse.
The urethra is a cylinder beneath the two large sponges that functions as a conduit to excrete urine waste and ejaculate sperm during intercourse. The urethra is surrounded by the corpus spongiosum, a smaller portion of sponge-type erection material that likewise becomes engorged during erection.
The tunica albuginea is a thick interwoven sheath of tissue that connects all of these sponges.
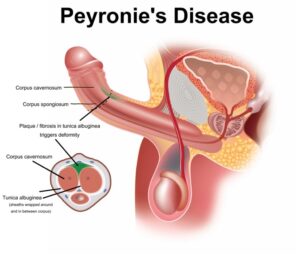
The penile plaque or fibrosis that causes Peyronie’s symptoms most usually forms somewhere along the tunica sheathing, although it can also form within and around the corpora sponge substance (intercorporeal or intracorporeal). As a result, Peyronie’s plaque or fibrosis have no effect on your capacity to urinate or ejaculate.
What is Peyronie’s disease?
Peyronie’s Disease Redefined
Peyronie’s Disease (PD) is an acquired inflammatory condition characterized by the buildup of fibrosis within the soft tissue of the penis and/or thickening of the tunica albuginea. In select cases, it’s triggered by a wound healing disorder.
Although a thicker tunica is infrequently included in previous Peyronie’s definitions, we discovered it to be prevalent enough to be included in our revised standard definition.
New ExoSurge® Peyronie’s Insight
Contrary to conventional wisdom often equating Peyronie’s and significant erect curvature as “synonymous”, we discovered roughly 35% of treated Peyronie’s patients started with little or no curve but always had a clear-cut Peyronie’s diagnosis from significant and measurable fibrosis and / or plaque in the penis.
The most common symptoms of Peyronie’s disease are curvature during erection, nodules3 you can feel with your fingertips just beneath the skin, misshaping of the penis, decrease in penile size, and rings or bands of differentiated tissue around or along the penile shaft, and erectile dysfunction.
[3] Chung E, De Young L, Brock GB. Penile duplex ultrasonography in men with Peyronie’s disease: is it veno-occlusive dysfunction or poor cavernosal arterial inflow that contributes to erectile dysfunction? J Sex Med. 2011;8(12):3446–3451
The French surgeon Francois De la Peyronie, personal physician to King Louis XV of France, made the first clinical diagnosis of Peyronie’s in 1743, however medical publications had been constantly mentioning the ailment as early as the 1400s. De la Peyronie, who also personally experienced the syndrome, proposed that it was brought on by sexual abuse-related chronic irritation as well as sexually transmitted diseases.
How common is Peyronie’s disease?
For years, Peyronie’s was estimated to be a low single digit’s incidence that was predominantly found in men over the age of 45-years-old.
The most oft quoted statistics regarding the prevalence of Peyronies was derived from Peyronie’s Disease, A Guide to Clinical Management by Levine4, published in 2007. Their studies show the condition increasing during the last 30 years and they estimated it to range between 3.7% and 7.1%. However, they indicated the actual prevalence might be substantially higher5 because of patients’ reluctance to report this embarrassing condition to physicians.
New ExoSurge® Peyronie’s Insight
Peyronie’s plaque is the first cousin of a benign tumor sharing close similarities in appearance, organic growth, and impact on the human body. As with the benign tumor, Peyronie’s fibrotic or plaque material can be visually measured from ultrasonography imagery in terms of existing dimensions, growth over time and/or reduction in size from treatment.
[4] Levine, L. A. (2007). Peyronie’s disease: A guide to clinical management. Totowa, NJ: Humana Press
[5] Smith BH.. Subclinical Peyronie’s disease. Am J Clin Pathol. 1969;52:385–390
A pair of recent studies6 which both garnered patients from the general populous and reduced the embarrassment associated with the indication showed a much larger prevalence of men with palpable plaque in the penis at about 13 % of the US male population7 or 14 million men.
Much higher indications for Peyronie’s are not without precedent. A 100-patient postmortem study8 by BH Smith in 1969 that examined the prevalence of fibrosis among cadavers disclosed a fibrosis incident rate of 23%. Additionally, a 1980 study from data derived from phalloarteriography by Michel9, et al found Peyronie’s deformity of 20%. Notably, most of the men where deformity was observed were aware they had any sort of problem. It’s also worth nothing Smith’s study occurred long before the sexual revolution, the proliferation of PGE injections to treat erectile dysfunction and other societal aspects that have increased the likelihood of penile injury.

[6] Dana Britt DiBenedetti, Dat Nguyen, Laurie Zografos, Ryan Ziemiecki, and Xiaolei Zhou, (2011) A Population-Based Study of Peyronie’s Disease: Pevalance and Treatment Patterns in the United States
[7] Stuntz M, Perlaky A, des Vignes F, Kyriakides T, Glass D (2016) The Prevalence of Peyronie’s Disease in the United States: A Population-Based Study. PLoS ONE 11(2): e0150157. doi:10.1371/journal.pone.0150157
[8] Smith BH. Subclinical Peyronie’s disease. Am J Pathol. 1969;52:385–90.
[9] Michal V, Posipichal J, Blazkova J . Arteriography of the internal pudendal arteries and passive erection In: Zorgniotti AW, Rossi G, eds Vasculogenic impotence Charles Thomas: Springfield Illinois 1980 pp 169–179
An impending Peyronie’s Disease prevalence explosion
Historical Peyronie’s Disease
prevalence studies among men age 30 and under showed a range10 in the low single digits between 1.0% and 3.5 %11 and even as low as 3.5% among men over the age of 5012.
However, a pair of recently released13 large prevalence studies now show the highest prevalence for men 18-24 (15%) and an elevated 14% among men 18-34 years old. This represents a 400% – 600% increase from historical norms. The current trend line among the under-45 crowd is equally alarming: the incidence rate is increasing 20% every five years.
Why such a big increase among younger men?
The situation has not been fully studied; however, we’ve found a much higher instances of young men with many of the Peyronie’s accelerators that are more commonly found in older males.
[10] Segundo, et al: Prevalence, Risk Factors, and Erectile Dysfunction Associated With Peyronie’s Disease Among Men Seeking Urological Care, Sexual Medicine Volume 8, Issue 2, June 2020, Pages 230-236
[11] Lindsay MB, Schain DM, Grambsch P, et al. The incidence of Peyronie’s disease in Rochester, Minnesota, 1950 through 1984. J Urol. 1991;146:1007–1009.
[12] Schwarzer U, Sommer F, Klotz T, et al. The prevalence of Peyronie’s disease: results of a large survey. BJU Int 2001; 88: 727–730.
[13] A. I. El-Sakka, “Prevalence of Peyronie’s disease among patients with erectile dysfunction,” European Urology, vol. 49, no. 3, pp. 564–569, 2006.
A future Peyronie’s epidemic?
If this incidence trend line is combined with the number of cases that will develop from acute penile trauma as a result of accidents, a future incidence rate of more than 20% of all men in the United States is a probable future reality.
Let’s consider the numbers:
- If the current increase in the number of Peyronie’s indications among younger men maintains currently evaluated levels (not maintaining the current 20% growth clip)
- The under-45 crowd numbers are combined with the new slightly higher percentage of men with PD 45 years and older
- We add a nominal allowable percentage (3%) for new PD diagnosis triggered by accidents and direct penile injury,
The result indicates 25-30% of adult US males could be facing consequences of penile fibrosis and plaques within the next 20 years.
We expect the permanent removal of the fibrosis and plaques associated with a Peyronie’s diagnosis to become a global challenge for the medical industry in the years ahead.
Chordee vs. Peyronie’s Disease: Which one do you have?
Are Peyronie’s disease and penile curvature the same thing?

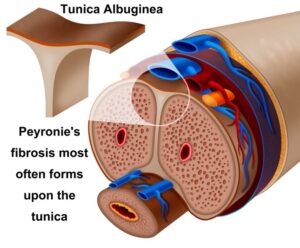
Peyronie’s Disease (PD) can cause curvature during erection depending upon the exact size, density and location of the penile fibrosis that triggers a Peyronie’s indication. Since most fibrosis associated with Peyronie’s imbeds itself in the tunica albuginea (the thick sheath that surrounds the functioning erectile tissue), a curvature during erection is a common side effect.
Some men are simply born with significant penile curvature. If you’ve had your curve since as long as you can recall when having erections, then you most likely have what’s called a “congenital curve” or chordee which is not a Peyronie’s diagnosis. You were born with this trait. Chordee affects approximately 1% of all men. There are reconstructive surgeries available to correct this curvature if it’s causing you problems with your sex life.
What causes penile curvature?
Non-Peyronie’s penile curvature is a natural, in-born trait. Most men have some sort of slight curve during erection, very few penises are 100% straight when erect.
Alas, with a congenital curvature, the degree of curve is more pronounced.
Penile curvature from Peyronie’s Disease is caused by buildup of fibrosis in the soft tissue of the penis which commonly creates curvature when the organ becomes engorged with blood during an erect state.
New ExoSurge® Peyronie’s Insight
During a breakout session among some of the best chordee surgeons in the US at the AUA convention in 2018, ExoSurge cofounder Kenneth J. Carney, MD was among a group that postulated that a congenital curve might occur when a penis grows faster than the body can accommodate its growth. They noted that practically all men with congenital curvature have a larger endowment than usual.
To date, no clinical investigations have been conducted to verify or contradict this idea.
How is penile curvature diagnosed?
Your urologist can quickly ascertain whether your curvature is congenital or Peyronie’s disease during a visit. For the evaluation, your doctor might administer a PGE injection to cause an erection.
It’s vital to remember that a patient can have both Peyronie’s disease in addition to a congenital curvature.
In fact, a patient with congenital curvature is more likely to have a Peyronie’s diagnosis since a penis might be more easily damaged during strenuous sexual activity if it is already significantly curved. In order to avoid “partner on top” during sex, it is advised for patients with chordee to pay attention to alignment.
Congenital curvature and Peyronie’s disease patients will have noted curvature when erect their entire lives, but they will notice the degree of curvature is growing. When erect, they may also experience pain where it had not previously been felt.
What are the symptoms of penile curvature?
A congenital curve is present from birth, whereas Peyronie’s curvature is brought on by trauma and the resulting accumulation of fibrosis in the penis, which causes the curvature. The fact that a congenital curvature has been present “for all long as they can recall” since early childhood is a prevalent characteristic among persons who have it.
How is penile curvature treated?
Unless your degree of curvature prevents you from engaging in sexual activity, the majority of urologists (including us) advise doing nothing and taking note to use caution when in close proximity.
In more egregious cases, reconstructive surgical intervention is advised. Surgery is used to shorten the penis to match the opposite side by making incisions along the non-curved shaft. This operation has a great success rate and is typically done without hospitalization.

